Tech Tonics Podcast: Sean Khozin, Attuned To Data Science
After escaping the revolution in Iran, Sean Khozin found his way to the United States, harmonizing his passion for patients and data into a career that’s led him into startups, the FDA, and most recently J&J, where he’s now Global Head of Data Strategy – all while pursuing his love of music.
The phrase “it’s complicated” tends to be overused, but it hardly seems to do justice to Sean’s journey. Sean was born in Tehran, a son sandwiched between two daughters. Life for Sean’s family changed after the Revolution; the arrest of his dad, a political scientist, suggested it might be a good time to emigrate, which the entire family eventually did. Sean, while in high school, initially went to live with relatives in Turkey, then came to the United States, where his family reunited in Maryland. Sean completed high school in the US, and attended the University of Maryland, studying neurobiology and music theory, and traveling extensively on the side to NYC to pursue his passion for music composition and performance (especially classical guitar).
After a pre-doctoral fellowship at the National Cancer Institute (NCI), and obtaining an MPH, Sean went to medical school, but was surprised by how unscientific so much of medicine was as compared to science. After receiving his MD, he took at detour into entrepreneurship for several years, before being seduced back into medicine, completing a fellowship in oncology at the NCI, drawn by the promise he could pursue sophisticated analytics, inspired by the intellectual activity that was occurring in DC at the time, in particular the work of Todd Park and Aneesh Chopra.
After his fellowship, Sean transitioned to the FDA, where he developed and championed the “INFORMED” initiative, which he’s described as “an incubator for driving innovations in agile technology, digital health, and data science to advance public health.” Late last year, Sean left DC for J&J, where he’s now head of data science strategy, and has the chance to work with some of the smartest and most decent people in the industry, including J&J’s head of R&D Mathai Mammen, (an MD/PhD classmate of David’s).
To listen to the show, please use the audio player below or find it on the Connected Social Media website or on iTunes.
We are delighted to welcome Sean to Tech Tonics!
Tech Tonics is grateful to Manatt Health for its sponsorship of the show.
The phrase “it’s complicated” tends to be overused, but it hardly seems to do justice to Sean’s journey. Sean was born in Tehran, a son sandwiched between two daughters. Life for Sean’s family changed after the Revolution; the arrest of his dad, a political scientist, suggested it might be a good time to emigrate, which the entire family eventually did. Sean, while in high school, initially went to live with relatives in Turkey, then came to the United States, where his family reunited in Maryland. Sean completed high school in the US, and attended the University of Maryland, studying neurobiology and music theory, and traveling extensively on the side to NYC to pursue his passion for music composition and performance (especially classical guitar).
After a pre-doctoral fellowship at the National Cancer Institute (NCI), and obtaining an MPH, Sean went to medical school, but was surprised by how unscientific so much of medicine was as compared to science. After receiving his MD, he took at detour into entrepreneurship for several years, before being seduced back into medicine, completing a fellowship in oncology at the NCI, drawn by the promise he could pursue sophisticated analytics, inspired by the intellectual activity that was occurring in DC at the time, in particular the work of Todd Park and Aneesh Chopra.
After his fellowship, Sean transitioned to the FDA, where he developed and championed the “INFORMED” initiative, which he’s described as “an incubator for driving innovations in agile technology, digital health, and data science to advance public health.” Late last year, Sean left DC for J&J, where he’s now head of data science strategy, and has the chance to work with some of the smartest and most decent people in the industry, including J&J’s head of R&D Mathai Mammen, (an MD/PhD classmate of David’s).
To listen to the show, please use the audio player below or find it on the Connected Social Media website or on iTunes.
We are delighted to welcome Sean to Tech Tonics!
Tech Tonics is grateful to Manatt Health for its sponsorship of the show.
CEO Rountable on Cancer: Maintaining Clinical Trial Integrity Amid COVID-19
Artificial Intelligence and Medical Imaging: Sean Khozin and Rob Califf
Autoimmune Disease and Immunotherapy Outcomes in Patients With NSCLC
ASCO Daily News
In an exploratory study using real-world data from electronic health records (EHRs), patients with advanced non−small cell lung cancer (NSCLC) and a history of autoimmune disease treated with immune checkpoint inhibitors (ICIs) had similar clinical outcomes compared with patients with no evidence of autoimmune disease (Abstract 110). There was, however, an increase in some types of immune-related adverse events (irAEs) that require further investigation, the study’s authors said.
These data were presented by Sean Khozin, MD, MPH, of the U.S. Food and Drug Administration, during the June 3 Clinical Science Symposium “Using Real-World Data to Advance Research and Care.” He explained that patients with autoimmune disease are typically excluded from traditional clinical trials, therefore there is little evidence supporting the use of ICIs in patients with advanced NSCLC who have a history of autoimmune disease. But anecdotal and early evidence suggest that, in real-world practice, ICIs are being used in routine care for patients with advanced NSCLC and a history of autoimmune disease.
This retrospective trial was designed to evaluate the real-world characteristics and outcomes of patients with advanced NSCLC, with or without a history of autoimmune disease, treated with ICIs in predominately community-based, U.S. oncology practices, and to explore irAEs in this population. The observational cohort study used de-identified EHR data from ASCO’s CancerLinQ® database, representing patient care in 49 diverse oncology practices. Data collection took place from January 2011 to November 2018.
Included in the study were adult patients diagnosed with advanced NSCLC who had received at least one dose of an ICI (ipilimumab, pembrolizumab, nivolumab, atezolizumab, durvalumab, or avelumab) and who had at least two documented clinical visits on or after the first administration of the ICI. Autoimmune disease status prior to ICI treatment was determined from EHRs based on ICD-9 or ICD-10 codes and autoimmune disease medications. Active autoimmune disease was defined as evidence of autoimmune disease in the year prior to starting the ICI.
Outcomes analyzed included time to treatment discontinuation (TTD), time to next treatment (TTNT), real-world progression-free survival (rwPFS), overall survival (OS), and irAEs.
From more than 1 million patients in the deidentified dataset, 2,402 patients who met the criteria were identified. Of those patients, autoimmune disease was present in 531. Most patient characteristics were similar between the cohorts, except that there was a higher percentage of women among the patients with history of autoimmune disease (54.6%) than in those with no evidence of it (43.5%).
In this real-world dataset, unlike in a clinical trial setting, there were notable percentages of patients with ECOG performance status of 2 or greater (16.9% of those with history of autoimmune disease and 14.4% of patients with no evidence of autoimmune disease).
Median OS in patients with autoimmune disease was 11.5 months (95% CI [9.63, 13.2]) and 12.8 months (95% CI [11.51, 14.2]) in patients with no autoimmune disease. TTD, TTNT, rwPFS, and OS did not differ between the two cohorts.
Although overall incidence of irAEs was not significantly different between the cohorts (27.1% in the autoimmune arm, 26.0% in the non-autoimmune arm), there were higher incidences of some types of irAEs among patients with autoimmune disease. These include blood and lymphatic (3.8% in the autoimmune arm vs. 2.4% in the non-autoimmune arm), endocrine (4.9% vs. 3.2%), gastrointestinal (8.9% vs. 7.6%), and general disorders (10.4% vs. 8.3%) irAEs. The study authors say this warrants further research to better understand how autoimmune disease impacts the incidence of irAEs.
“Our findings supplement previous exploratory analyses based on very limited clinical trial data suggesting the relative safety of the use of ICIs in patients with a history of autoimmune disease,” Dr. Khozin said.
Discussant David E. Kozono, MD, PhD, of Dana-Farber Cancer Institute, commented that “Dr. Khozin and colleagues showed us an excellent example of the use of real-world data to identify outcomes in an uncommon population”—that is, patients with cancer and autoimmune disease. This is an important area to explore, he said, because irAEs related to ICIs largely affect the same organs that are impacted by autoimmune disease, giving credence to concerns that ICIs may exacerbate it.
– Tim Donald, ELS
Presidential Innovation Fellows Join FDA to Advance Digital Health
A new team of Presidential Innovation Fellows (PIF), Robert Goldel and Rana Saad, have begun their work at the Food and Drug Administration (FDA), applying data science approaches to device, drug, and software development, and the associated regulatory decisions.
Project teams at the agency have been exploring ways to incorporate more digital tools into its own processes within the FDA, including the drug approval process. The FDA has also been reviewing how, through the software precertification pilot program, to streamline processes for reviewing digital technology that are medical devices.
“The FDA has committed to being at the forefront of advancing the use of digital tools to empower consumers to take an active role in managing their own health while creating new opportunities for the agency to carry out its public health mission, such as through improved measurement of important endpoints in clinical trials and ensuring patients have access to safe, effective digital health devices,” said Dr. Sean Khozin, Director of FDA’s INFORMED. “We’re also looking at ways to incorporate more advanced digital processes into our regulatory review process, through INFORMED and other efforts. We’re excited to be working with the Presidential Innovation Fellows and to apply their experiences to enhance and scale our digital health strategy and research portfolio.”
Robert Goldel will be working closely with Dr. Sean Khozin, the Founding Director of INFORMED on questions of digital biomarkers, artificial intelligence (AI), and machine learning approaches in medicine. Khozin and Goldel will also be coordinating and supporting FDA work groups establishing data science and algorithm / AI regulations, procedures, and programs that have national or international impact.
“I am deeply honored to receive this Presidential Innovation Fellowship,” says Robert Goldel. “As a neuroscientist and data-driven technologist I’m really excited to be joining the FDA to promote and protect public health. I’m humbled to support their digital efforts by drawing from my experiences in neuroscience, biosensors, mobile and cloud software, artificial intelligence, and machine learning.”
Goldel believes the potential to link these technologies with traditional approaches in foods, medical devices, and pharmaceuticals is where personalized medicine is headed. “I’m looking forward to learning from the amazing people and history at the FDA. The future of digital health depends upon their expertise and passion to ensure the regulatory frameworks for software as medicine and the wide diversity of new technologies,” Goldel adds.
Rana Saad will be working closely with Mr. Bakul Patel, Associate Director for Digital Health in the FDA’s Center for Devices and Radiological Health, on standing up the infrastructure and organization needed for the Digital Health Unit at the FDA that is responsible for the software Pre-Certification pilot program (Pre-Cert) – which is going to help develop an innovative regulatory paradigm which will be designed to maximize safety of medical devices while matching the speed of innovation to realize the full potential of digital health technologies. Patel and Saad will also be coordinating and supporting the FDA to build its bench strength to prepare to be digital future ready.
“This is an exciting, pivotal time to join the FDA,” said Saad. “There is tremendous opportunity to positively impact millions of lives through working with the FDA’s staff to develop policies for regulating digital innovations in healthcare in general. It will be wonderful to play a role in helping accelerate the pace of innovation in this important area.”
Project teams at the agency have been exploring ways to incorporate more digital tools into its own processes within the FDA, including the drug approval process. The FDA has also been reviewing how, through the software precertification pilot program, to streamline processes for reviewing digital technology that are medical devices.
“The FDA has committed to being at the forefront of advancing the use of digital tools to empower consumers to take an active role in managing their own health while creating new opportunities for the agency to carry out its public health mission, such as through improved measurement of important endpoints in clinical trials and ensuring patients have access to safe, effective digital health devices,” said Dr. Sean Khozin, Director of FDA’s INFORMED. “We’re also looking at ways to incorporate more advanced digital processes into our regulatory review process, through INFORMED and other efforts. We’re excited to be working with the Presidential Innovation Fellows and to apply their experiences to enhance and scale our digital health strategy and research portfolio.”
Robert Goldel will be working closely with Dr. Sean Khozin, the Founding Director of INFORMED on questions of digital biomarkers, artificial intelligence (AI), and machine learning approaches in medicine. Khozin and Goldel will also be coordinating and supporting FDA work groups establishing data science and algorithm / AI regulations, procedures, and programs that have national or international impact.
“I am deeply honored to receive this Presidential Innovation Fellowship,” says Robert Goldel. “As a neuroscientist and data-driven technologist I’m really excited to be joining the FDA to promote and protect public health. I’m humbled to support their digital efforts by drawing from my experiences in neuroscience, biosensors, mobile and cloud software, artificial intelligence, and machine learning.”
Goldel believes the potential to link these technologies with traditional approaches in foods, medical devices, and pharmaceuticals is where personalized medicine is headed. “I’m looking forward to learning from the amazing people and history at the FDA. The future of digital health depends upon their expertise and passion to ensure the regulatory frameworks for software as medicine and the wide diversity of new technologies,” Goldel adds.
Rana Saad will be working closely with Mr. Bakul Patel, Associate Director for Digital Health in the FDA’s Center for Devices and Radiological Health, on standing up the infrastructure and organization needed for the Digital Health Unit at the FDA that is responsible for the software Pre-Certification pilot program (Pre-Cert) – which is going to help develop an innovative regulatory paradigm which will be designed to maximize safety of medical devices while matching the speed of innovation to realize the full potential of digital health technologies. Patel and Saad will also be coordinating and supporting the FDA to build its bench strength to prepare to be digital future ready.
“This is an exciting, pivotal time to join the FDA,” said Saad. “There is tremendous opportunity to positively impact millions of lives through working with the FDA’s staff to develop policies for regulating digital innovations in healthcare in general. It will be wonderful to play a role in helping accelerate the pace of innovation in this important area.”
Real World Endpoints with Sean Khozin
Flatiron Inaugural Research Summit
Dr. Khozin proposes a framework for contextualizing the many endpoints available to researchers working with real-world data. Rather than holding each endpoint to the same standard, he proposed thinking about them in three categories: “validated”, “reasonably likely”, and “candidate”. While many real-world endpoints fall into the “candidate” category, he acknowledges that endpoints in the middle category – “reasonably likely” (e.g. Response Rate) – may be suitable for use in accelerated approvals.
Dr. Khozin proposes a framework for contextualizing the many endpoints available to researchers working with real-world data. Rather than holding each endpoint to the same standard, he proposed thinking about them in three categories: “validated”, “reasonably likely”, and “candidate”. While many real-world endpoints fall into the “candidate” category, he acknowledges that endpoints in the middle category – “reasonably likely” (e.g. Response Rate) – may be suitable for use in accelerated approvals.
Leveraging Real-World Evidence for Regulatory Use
Flatiron Inaugural Research Summit
with Drs. Khozin, Miksad, and Abernethy
The interest in real‐world evidence in a regulatory context is rapidly growing. Recent advances in data quality and experience with appropriate regulatory use cases are crucial steps towards effective use of RWE for regulatory decision-making.
with Drs. Khozin, Miksad, and Abernethy
The interest in real‐world evidence in a regulatory context is rapidly growing. Recent advances in data quality and experience with appropriate regulatory use cases are crucial steps towards effective use of RWE for regulatory decision-making.
Precision Medicine: Clinicogenomic Database
Starts here (2:14)
PRecompetitive use of algorithms (National Academies)
Data Standardization and Harmonization (National Academies)
The Future of Real world Evidence
INFORMED: An Interview with Sean Khozin, MD, MPH
The Information Exchange and Data Transformation (INFORMED) initiative was launched by the U.S. Food and Drug Administration (FDA) and the Innovation, Design, Entrepreneurship and Action (IDEA) Lab of the U.S. Department of Health and Human Services. INFORMED is intended to promote the use of big data analytics to analyze the large and disparate clinical evidence now available to researchers and regulators. Sean Khozin, MD, MPH, Acting Associate Director, Oncology Regulatory Science and Informatics at the FDA’s Oncology Center of Excellence and a founder of INFORMED, discussed the details of the initiative for IASLC Lung Cancer News readers.
What are the goals of INFORMED?
The primary goal of INFORMED is to expand and maintain organizational and technical infrastructure for big data analytics. This is done by functioning as an incubator for conducting collaborative regulatory science research focused on supporting innovations that enhance FDA’s mission of promotion and protection of public health.
Organizationally, INFORMED is serving as a sandbox, where we’ve paired new talent such as entrepreneurs-in-residence, engineers, and data scientists with subject matter experts such as oncologists at the FDA. The synergy we’ve created among groups with complementary skill sets is quite unique and has been very productive. We’re also continuously building and expanding robust technical infrastructure through internal agile software development and pilots with the technology groups, such as Palantir, at the leading edge of big data aggregation and analytics.
How has the development of precision medicine changed the process of drug development in the field of oncology?
As we all know, precision medicine is defined as the right therapy delivered to the right patient at the right time and in the right dose. The idea of precision medicine is driving the healthcare and drug development industry from a population health outlook to a patient-centered approach: holistic and individualized, as opposed to reductionist and generalized. A holistic approach considers a variety of intrinsic (e.g., genomic and proteomic) and extrinsic (e.g., environmental) variables in making drug development and treatment decisions that are tailored to the individual, not an entire population of patients as defined by traditional diagnostic terms and traditional clinical trial designs. For example, in the past decade, we’ve recognized that not all non-small cell lung cancer (NSCLC) patients have the same kind of disease, as we discovered mutations and translocations such as EGFR and ALK that greatly influence response to therapy and outcomes. Some molecular aberrations in NSCLC, such as BRAF and ROS1, occur in less than 2% of patients and when combined with other intrinsic and extrinsic variables, we end up with very small cohorts and in some cases N of 1s.
Developing drugs and delivering care that is precisely tailored to small groups and individual patients requires fundamental changes in how we approach drug discovery, clinical evidence generation, and healthcare delivery. It requires us to capture and analyze big data sets from traditional (e.g., conventional clinical trials) and novel pipelines (e.g., realworld data and biometric sensors), using new study designs to better understand the patient’s experience in the context of a sustainable framework for precision delivery of therapies and healthcare services.
What types of organizations and researchers participate in INFORMED?
As an incubator, INFORMED conducts collaborative research with innovators in professional organizations, academia, nonprofits, and industry. For example, in the domain of real-world evidence generation, we have research collaborations with the American Society of Clinical Oncology’s CancerLinQ and a start-up called Flatiron Health. In the area of data sharing, we’re collaborating with a nonprofit called Project Data Sphere on open access data. We are also developing a framework for decentralized sharing of data at scale with IBM Watson Health based on blockchain, which allows users to access and add to a secure, shared ledger or spreadsheet of data. We’re also working with data science experts at MIT and Stanford on innovations based on artificial intelligence and algorithmic analytics that can help the drug development and the life sciences communities.
What is “systems thinking” and why is it emphasized in the INFORMED initiative
Systems thinking is a prerequisite for enabling precision medicine and, as a theoretical foundation, can be an optimal framework for making regulatory decisions. Traditional sciences are largely siloed into specific disciplines and not organically designed as multidisciplinary units. Progress in traditional sciences is characterized by intense specialization into specific disciplinary boundaries. In contrast, regulatory science, which is what INFORMED is all about, takes a systems science view of the world, where the focus is on networks and relationships, and where progress is best characterized by becoming more inclusive and holistic, as opposed to being specialized into narrowly defined fields. By quantifying networks and interconnected relationships, from the molecular level (e.g., systems biology) to the macro scale (e.g., market dynamics), systems thinking can allow for objective and data-driven regulatory decision-making in order to have the greatest positive impact on public health.
What should clinicians know about the INFORMED project?
INFORMED is a translational incubator at the intersection of data science, health tech, and the life sciences. The aim, however, is not technology for the sake of technology: we use advanced tools and methods to help diffuse innovations into the point of care by catalyzing the development and adoption of precision tools and therapeutics. Our systems view of the ecosystem is not about the system itself, but about enabling appropriate treatment decisions locally, where care is delivered. Therefore, empowering physicians and other healthcare providers is one of the focal points of our efforts, and we welcome and depend on their continued input and participation as the pillars of the healthcare delivery system.✦
What are the goals of INFORMED?
The primary goal of INFORMED is to expand and maintain organizational and technical infrastructure for big data analytics. This is done by functioning as an incubator for conducting collaborative regulatory science research focused on supporting innovations that enhance FDA’s mission of promotion and protection of public health.
Organizationally, INFORMED is serving as a sandbox, where we’ve paired new talent such as entrepreneurs-in-residence, engineers, and data scientists with subject matter experts such as oncologists at the FDA. The synergy we’ve created among groups with complementary skill sets is quite unique and has been very productive. We’re also continuously building and expanding robust technical infrastructure through internal agile software development and pilots with the technology groups, such as Palantir, at the leading edge of big data aggregation and analytics.
How has the development of precision medicine changed the process of drug development in the field of oncology?
As we all know, precision medicine is defined as the right therapy delivered to the right patient at the right time and in the right dose. The idea of precision medicine is driving the healthcare and drug development industry from a population health outlook to a patient-centered approach: holistic and individualized, as opposed to reductionist and generalized. A holistic approach considers a variety of intrinsic (e.g., genomic and proteomic) and extrinsic (e.g., environmental) variables in making drug development and treatment decisions that are tailored to the individual, not an entire population of patients as defined by traditional diagnostic terms and traditional clinical trial designs. For example, in the past decade, we’ve recognized that not all non-small cell lung cancer (NSCLC) patients have the same kind of disease, as we discovered mutations and translocations such as EGFR and ALK that greatly influence response to therapy and outcomes. Some molecular aberrations in NSCLC, such as BRAF and ROS1, occur in less than 2% of patients and when combined with other intrinsic and extrinsic variables, we end up with very small cohorts and in some cases N of 1s.
Developing drugs and delivering care that is precisely tailored to small groups and individual patients requires fundamental changes in how we approach drug discovery, clinical evidence generation, and healthcare delivery. It requires us to capture and analyze big data sets from traditional (e.g., conventional clinical trials) and novel pipelines (e.g., realworld data and biometric sensors), using new study designs to better understand the patient’s experience in the context of a sustainable framework for precision delivery of therapies and healthcare services.
What types of organizations and researchers participate in INFORMED?
As an incubator, INFORMED conducts collaborative research with innovators in professional organizations, academia, nonprofits, and industry. For example, in the domain of real-world evidence generation, we have research collaborations with the American Society of Clinical Oncology’s CancerLinQ and a start-up called Flatiron Health. In the area of data sharing, we’re collaborating with a nonprofit called Project Data Sphere on open access data. We are also developing a framework for decentralized sharing of data at scale with IBM Watson Health based on blockchain, which allows users to access and add to a secure, shared ledger or spreadsheet of data. We’re also working with data science experts at MIT and Stanford on innovations based on artificial intelligence and algorithmic analytics that can help the drug development and the life sciences communities.
What is “systems thinking” and why is it emphasized in the INFORMED initiative
Systems thinking is a prerequisite for enabling precision medicine and, as a theoretical foundation, can be an optimal framework for making regulatory decisions. Traditional sciences are largely siloed into specific disciplines and not organically designed as multidisciplinary units. Progress in traditional sciences is characterized by intense specialization into specific disciplinary boundaries. In contrast, regulatory science, which is what INFORMED is all about, takes a systems science view of the world, where the focus is on networks and relationships, and where progress is best characterized by becoming more inclusive and holistic, as opposed to being specialized into narrowly defined fields. By quantifying networks and interconnected relationships, from the molecular level (e.g., systems biology) to the macro scale (e.g., market dynamics), systems thinking can allow for objective and data-driven regulatory decision-making in order to have the greatest positive impact on public health.
What should clinicians know about the INFORMED project?
INFORMED is a translational incubator at the intersection of data science, health tech, and the life sciences. The aim, however, is not technology for the sake of technology: we use advanced tools and methods to help diffuse innovations into the point of care by catalyzing the development and adoption of precision tools and therapeutics. Our systems view of the ecosystem is not about the system itself, but about enabling appropriate treatment decisions locally, where care is delivered. Therefore, empowering physicians and other healthcare providers is one of the focal points of our efforts, and we welcome and depend on their continued input and participation as the pillars of the healthcare delivery system.✦
Digital Footprints in Drug Development
FAST Company: Dr. Jay Parkinson and Dr. Sean Khozin offer a glimpse of hassle-free health care
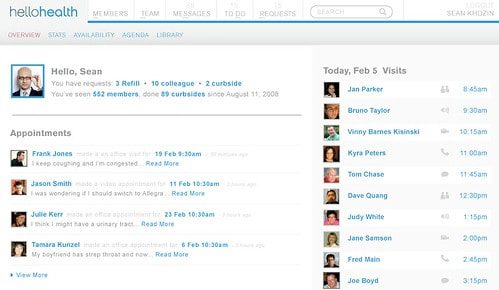
Myca and Hello Health Preview Their Facebook-like Medical Platform
Today in Boston, at Health 2.0, Dr. Jay Parkinson and Dr. Sean Khozin offer a glimpse of hassle-free health care
By Chuck Salter
As we explored this month in “The Doctor of the Future,” the doctor-patient relationship isn’t what it used to be. Take primary-care physicians. Because insurance companies pay them considerably less than specialists, they rely on volume. The more office visits these docs can squeeze in, the more procedures they can perform and bill for. But getting paid by tight-fisted insurers requires a tenacious staff to file endless paperwork and engage in the reimbursement dance of procedural codes and multiple phone calls.
Today in Boston, at the Health 2.0 conference, which focuses on innovative health care, Dr. Jay Parkinson and Dr. Sean Khozin of Hello Health in Brooklyn unveil a different kind of medical practice. Paradoxically, it allows them to devote more time and attention to patients by often employing remote medicine.
A few weeks ago, Parkinson, an inveterate blogger and the chief concept officer at the software company Myca, gave me a sneak preview of the platform. It’s part electronic medical record, part practice-management system, and part social-networking site, complete with profiles and photos of doctors and patients, all in a secure environment that complies with federal privacy standards. Unlike traditional electronic medical records, which are designed primarily to facilitate billing, this application is primarily about enhancing communication–between doctors and patients, as well as among doctors.
Your patient home page displays your medical team, which includes your primary-care physician and any specialists. You choose them by location or patient ratings, or go with the experts listed on your primary-care physician’s profile. To schedule an appointment, you simply pull up a doctor’s schedule, select a half hour or hour time slot, and indicate the type of appointment–in-person, video chat, email, etc. You also describe your complaint in a text box, which allows the doctor to think about the issue beforehand. After the appointment, you–and your doctor–can review the visit, a smart solution to avoid forgetting what was said. That alone could lead to dramatically improved care.
Joining the Myca platform is free; doctors set their own fees per visit, and Myca gets a cut. “It’s like Zipcar, but instead of renting a car, you’re renting a doctor,” says Parkinson.
True, all the kinks have yet to be worked out. Insurance companies, for instance, haven’t fully embraced e-visits yet, but they’re beginning to cover them. It feels like it’s only a matter of time, though. Patients–and their doctors–will soon expect and demand this kind of convenience and access.
Today in Boston, at Health 2.0, Dr. Jay Parkinson and Dr. Sean Khozin offer a glimpse of hassle-free health care
By Chuck Salter
As we explored this month in “The Doctor of the Future,” the doctor-patient relationship isn’t what it used to be. Take primary-care physicians. Because insurance companies pay them considerably less than specialists, they rely on volume. The more office visits these docs can squeeze in, the more procedures they can perform and bill for. But getting paid by tight-fisted insurers requires a tenacious staff to file endless paperwork and engage in the reimbursement dance of procedural codes and multiple phone calls.
Today in Boston, at the Health 2.0 conference, which focuses on innovative health care, Dr. Jay Parkinson and Dr. Sean Khozin of Hello Health in Brooklyn unveil a different kind of medical practice. Paradoxically, it allows them to devote more time and attention to patients by often employing remote medicine.
A few weeks ago, Parkinson, an inveterate blogger and the chief concept officer at the software company Myca, gave me a sneak preview of the platform. It’s part electronic medical record, part practice-management system, and part social-networking site, complete with profiles and photos of doctors and patients, all in a secure environment that complies with federal privacy standards. Unlike traditional electronic medical records, which are designed primarily to facilitate billing, this application is primarily about enhancing communication–between doctors and patients, as well as among doctors.
Your patient home page displays your medical team, which includes your primary-care physician and any specialists. You choose them by location or patient ratings, or go with the experts listed on your primary-care physician’s profile. To schedule an appointment, you simply pull up a doctor’s schedule, select a half hour or hour time slot, and indicate the type of appointment–in-person, video chat, email, etc. You also describe your complaint in a text box, which allows the doctor to think about the issue beforehand. After the appointment, you–and your doctor–can review the visit, a smart solution to avoid forgetting what was said. That alone could lead to dramatically improved care.
Joining the Myca platform is free; doctors set their own fees per visit, and Myca gets a cut. “It’s like Zipcar, but instead of renting a car, you’re renting a doctor,” says Parkinson.
True, all the kinks have yet to be worked out. Insurance companies, for instance, haven’t fully embraced e-visits yet, but they’re beginning to cover them. It feels like it’s only a matter of time, though. Patients–and their doctors–will soon expect and demand this kind of convenience and access.
Hello Health, Goodbye Hassle
In the heart of Hipsterville, New York (that’s Williamsburg, Brooklyn) you’d expect to find microbreweries like the Brooklyn Brewery and trendy children’s clothing stores like Smoochie Baby. Within walking distance of both, however, you can also find Hello Health, a cutting-edge medical practice that doesn’t accept insurance but does offer instant messaging, email, video conferencing, and secure electronic medical records to its members.
Hello Health reflects the antiestablishment ethos that pervades Williamsburg. Dr. Sean Khozin, one of its founding doctors, explains that the practice was built on a conscious decision to drop out of the existing health-care payment system, which he believes drives up costs and strangles innovation.
“A lot of the stuff that physicians do today has nothing to do with delivering quality care,” he says. “It’s just paperwork to satisfy the needs of third parties—mainly insurers—that are outside the doctor-patient relationship. There isn’t any other profession where ‘third parties’ dictate so much what you can and cannot do. Most practicing physicians spend over 30 percent of their administrative costs just dealing with insurance companies—and that’s outside of any other costs they may have, like medical malpractice insurance.”
After graduating from medical school, Khozin quickly became discouraged by the depressing reality of day-to-day clinical practice. Primary-care physicians face low reimbursements from insurers and must navigate reams of red tape just to get paid. To compensate, they see dozens of patients every day, spending just a few minutes with each. Given the poor working conditions, many doctors opt for early retirement or more lucrative specialties, generating a national shortage of primary-care doctors. That shortage is bound to get worse, thanks to the millions of uninsured patients who will enter the system if, as seems likely, Congress passes legislation mandating that individuals buy health insurance.
Doctors aren’t the only ones feeling frustrated. It’s not uncommon for patients to wait weeks for an appointment with their physician, sit for hours in the doctor’s lobby, and then stutter out a few symptoms before the doctor disappears again, a blur in a lab coat.
Khozin turned to research and medical communications after completing his post-medical-school residency (he also has a degree in public health). He never lost his interest in helping patients or finding a better way to practice medicine. Eventually, he developed a partnership with Myca, a Canadian technology company, and launched Hello Health as a demonstration project. He aimed to create a new business model for medicine, “direct care,” that uses the Internet and social networking tools like email and instant messaging (IM) to connect doctors with patients while bypassing insurers and bureaucrats. Patients can search for doctors, find services and fees, and make appointments on the Hello Health website. Because they don’t accept insurance and use technology to streamline processes, Hello Health physicians have much lower overhead and can pass the savings on to patients. For instance, Khozin charges $35 a month for membership and $125 for office and video visits. Quick emails, texts, and IMs are free, as are some simple lab tests and up to two months’ worth of prescriptions for generic drugs. Other physicians using Hello Health can set their own patient-friendly fee schedules.
Hello Health appeals to patients who are uninsured or underinsured and need access to basic, affordable health care, or who have Health Savings Accounts coupled with a high-deductible health plan that covers catastrophic costs. HSAs allow patients to pay for routine costs out-of-pocket, encouraging them to shop for the best health-care values. Khozin is a big fan of the HSA model. “I think everyone should have catastrophic insurance, but let the market take care of routine care, which can be very cheap.”
The current system’s perverse incentives can lead to overutilization of expensive (and well-reimbursed) services that don’t lead to better outcomes and may even hurt some patients by exposing them to needless risks and side effects. “One of the main problems driving U.S. health care costs out of control is the fragmentation of care,” Khozin says. “Doctors are paid on a fee-for-service basis, not for diagnosing or managing illnesses to achieve better outcomes at lower cost.” Because Khozin and his colleagues get paid for their services in full at every session, they have no incentive to do anything more—or less—than what they think is in the best interest of their patients.
President Obama and many health-care experts like to hold up the Mayo Clinic as an example of the high-quality, low-cost, integrated-care model that the rest of the country should follow. At the Mayo Clinic, doctors work in teams and are paid in annual salaries rather than fee-for-service. But most physicians actually work in small practices (often with just two or three doctors), and it’s just too impractical and expensive to expect all of them suddenly to join large integrated practices
The Myca technology platform solves that problem by allowing primary-care physicians and specialists who don’t share the same offices to view patients’ health records in real time, discuss the patients’ history through email or IM, and ensure that care remains coordinated. “We’ve created true continuity of care,” Khozin notes, “and strengthened the doctor-patient relationship, which, at the end of the day, is what chronic care management is all about.” Technology also improves care management by putting doctors and patients in regular communication and enabling doctors to monitor their patients’ progress and make recommendations that can improve outcomes.
Will the Hello Health model survive the health-care legislation winding its way through Congress? Khozin is cautiously optimistic: “We need to find different ways of delivering care, and the direct-care model we’re developing is one of the most viable ways to fix the primary-care system.”
Regulators and policymakers have a lot to learn from what physicians like Khozin are doing. Rather than trying to dictate health-care arrangements from the top down, innovators like Hello Health are creating and bundling services that patients want and can afford. That’s about as hip as it gets, in Brooklyn or anywhere else.
Paul Howard is director of the Manhattan Institute’s Center for Medical Progress.
Hello Health reflects the antiestablishment ethos that pervades Williamsburg. Dr. Sean Khozin, one of its founding doctors, explains that the practice was built on a conscious decision to drop out of the existing health-care payment system, which he believes drives up costs and strangles innovation.
“A lot of the stuff that physicians do today has nothing to do with delivering quality care,” he says. “It’s just paperwork to satisfy the needs of third parties—mainly insurers—that are outside the doctor-patient relationship. There isn’t any other profession where ‘third parties’ dictate so much what you can and cannot do. Most practicing physicians spend over 30 percent of their administrative costs just dealing with insurance companies—and that’s outside of any other costs they may have, like medical malpractice insurance.”
After graduating from medical school, Khozin quickly became discouraged by the depressing reality of day-to-day clinical practice. Primary-care physicians face low reimbursements from insurers and must navigate reams of red tape just to get paid. To compensate, they see dozens of patients every day, spending just a few minutes with each. Given the poor working conditions, many doctors opt for early retirement or more lucrative specialties, generating a national shortage of primary-care doctors. That shortage is bound to get worse, thanks to the millions of uninsured patients who will enter the system if, as seems likely, Congress passes legislation mandating that individuals buy health insurance.
Doctors aren’t the only ones feeling frustrated. It’s not uncommon for patients to wait weeks for an appointment with their physician, sit for hours in the doctor’s lobby, and then stutter out a few symptoms before the doctor disappears again, a blur in a lab coat.
Khozin turned to research and medical communications after completing his post-medical-school residency (he also has a degree in public health). He never lost his interest in helping patients or finding a better way to practice medicine. Eventually, he developed a partnership with Myca, a Canadian technology company, and launched Hello Health as a demonstration project. He aimed to create a new business model for medicine, “direct care,” that uses the Internet and social networking tools like email and instant messaging (IM) to connect doctors with patients while bypassing insurers and bureaucrats. Patients can search for doctors, find services and fees, and make appointments on the Hello Health website. Because they don’t accept insurance and use technology to streamline processes, Hello Health physicians have much lower overhead and can pass the savings on to patients. For instance, Khozin charges $35 a month for membership and $125 for office and video visits. Quick emails, texts, and IMs are free, as are some simple lab tests and up to two months’ worth of prescriptions for generic drugs. Other physicians using Hello Health can set their own patient-friendly fee schedules.
Hello Health appeals to patients who are uninsured or underinsured and need access to basic, affordable health care, or who have Health Savings Accounts coupled with a high-deductible health plan that covers catastrophic costs. HSAs allow patients to pay for routine costs out-of-pocket, encouraging them to shop for the best health-care values. Khozin is a big fan of the HSA model. “I think everyone should have catastrophic insurance, but let the market take care of routine care, which can be very cheap.”
The current system’s perverse incentives can lead to overutilization of expensive (and well-reimbursed) services that don’t lead to better outcomes and may even hurt some patients by exposing them to needless risks and side effects. “One of the main problems driving U.S. health care costs out of control is the fragmentation of care,” Khozin says. “Doctors are paid on a fee-for-service basis, not for diagnosing or managing illnesses to achieve better outcomes at lower cost.” Because Khozin and his colleagues get paid for their services in full at every session, they have no incentive to do anything more—or less—than what they think is in the best interest of their patients.
President Obama and many health-care experts like to hold up the Mayo Clinic as an example of the high-quality, low-cost, integrated-care model that the rest of the country should follow. At the Mayo Clinic, doctors work in teams and are paid in annual salaries rather than fee-for-service. But most physicians actually work in small practices (often with just two or three doctors), and it’s just too impractical and expensive to expect all of them suddenly to join large integrated practices
The Myca technology platform solves that problem by allowing primary-care physicians and specialists who don’t share the same offices to view patients’ health records in real time, discuss the patients’ history through email or IM, and ensure that care remains coordinated. “We’ve created true continuity of care,” Khozin notes, “and strengthened the doctor-patient relationship, which, at the end of the day, is what chronic care management is all about.” Technology also improves care management by putting doctors and patients in regular communication and enabling doctors to monitor their patients’ progress and make recommendations that can improve outcomes.
Will the Hello Health model survive the health-care legislation winding its way through Congress? Khozin is cautiously optimistic: “We need to find different ways of delivering care, and the direct-care model we’re developing is one of the most viable ways to fix the primary-care system.”
Regulators and policymakers have a lot to learn from what physicians like Khozin are doing. Rather than trying to dictate health-care arrangements from the top down, innovators like Hello Health are creating and bundling services that patients want and can afford. That’s about as hip as it gets, in Brooklyn or anywhere else.
Paul Howard is director of the Manhattan Institute’s Center for Medical Progress.
Docs Say Goodbye to Bureaucracy, Hello Health
With the debate over President Barack Obama's healthcare reform bill raging on Capitol Hill, some physicians are carving out their own path to reform that involves eliminating barriers to care and improving the doctor-patient relationship through the use of technology.
"The health system has been moving in the wrong direction," says Sean Khozin, MD, MPH. "People talk about healthcare reform, but no one is talking about what happens between a doctor and a patient. We have to pay much closer attention to the way that doctors and patients interact and transact and enhance that process because that's where care is delivered."
Khozin's futuristic Brooklyn, NY-based practice is unlike any other. It is powered by Hello Health, a secure, Web-based platform that includes a practice management system, an electronic medical records system, and a social networking tool that allows physicians to communicate with patients both online and face-to-face. Another Hello Health practice is scheduled to open in the West Village. Both practices serve as the beta testing grounds for the product, which was developed in collaboration with a Quebec-based technology company called Myca.
Creating improved access to care
After a patient establishes a relationship with a Hello Health doctor, he or she can use e-mail, video chat, instant messaging, or phone to reach their physician to ask questions, obtain test results, and to conduct other matters which would typically require an appointment in the office.
"We establish a relationship with a patient and we do a lot of the follow ups and care coordination online," says Khozin. "We cut down on the number of unnecessary visits while giving patients different channels of communication with their doctor."
Patients still have the option of scheduling an appointment if they have a problem that requires attention, but he has found that most of the time he can conduct patient follow up visits remotely.
While not all patients feel comfortable using technology to communicate with their physicians, Khozin says they learn over time and with his encouragement. He expects that more and more people will begin relying on technology to communicate with healthcare professionals.
While video-chatting with your physician may sound out of the ordinary now, Khozin predicts that it a few years it will be commonplace for a large segment of the population. In fact, today's young generation will more than likely expect this type of communication in the future because of the way that they have embraced technology and integrated it into their lives.
For example, the company is conscious of how popular smart phones have become. According to an April report by Manhattan Research, the number of physicians using smart phones more than doubled to 64% over the past year. In response to this growing trend, the company is in the process of developing applications for use on the Apple iPhone to address the needs of patients and physicians who want to communicate using smart phones.
"A smart, health IT company builds products for devices that people already have."
Khozin currently uses his iPhone to e-prescribe, review test results, e-mail, and graph and trend disease information for patients while they are in the office.
He says that with diabetes and heart disease on the rise, physicians need to engage patients and pull them into the process of care by allowing them to use online tools to better track their health and communicate information remotely.
For example, patients with diabetes would be able to submit their glucose levels online to Hello Health and have their physician monitor their results and respond to them if necessary—all without an office appointment.
"We can't rely on office visits alone anymore," he says. "Even if you have a chronic disease and you see your doctor four times a year, the rest of the time you're on your own. By connecting a doctor virtually with a patient, you can ensure continuity of care."
Building a Hello Health "ecosystem"
When physicians conduct an in-office or remote transaction with a patient, it automatically becomes part of that patient's electronic medical record in the Hello Health platform. The patient can view their medical record at any time. In addition, other physicians in the practice who see the patient and have access to the system can also view the same information.
The company plans to develop regional "ecosystems" on the Hello Health platform that will consist of a group of primary care doctors and specialists who can communicate with the patient and with one another in a patient-centered environment. Khozin says that specialists are beginning to participate in the Hello Health platform in New York and he expects similar ecosystems to be launched throughout the country.
"There's a lot of ways this technology can be implemented in terms of coordinating the care of complex patients, such as cancer patients," he says. "It's so difficult to really take care of these patients because of lack of access to the right information when you need it."
An elegant platform to replace Frankenstein systems
L. Gordon Moore, MD, a family medicine physician, has been waiting for a product like Hello Health to come along for quite some time. He is credited with pioneering the Ideal Medical Practice (IMP) philosophy. Physicians who subscribe to IMP concepts operate low-overhead, high-technology practices that provide patient-centered care that is efficient, effective, and accessible.
To run these types of practices, physicians often piece together many different pieces of technology to build a grassroots version of what Hello Health now offers. They pull together billing systems, appointment schedulers, and bare bones EMR applications to come up with a complete, albeit imperfect, package.
"Other docs have picked up this Frankenstein system, and it's hard," he says. "They're pouring money into IT to finesse this Holy Grail of interoperability, which is almost an illusion."
By comparison, Moore describes Hello Health as an "elegant platform." "It manages relationships like nothing I've ever seen," he says. "It's really the best IT solution that I've seen out there so far."
Moore is in the process of developing Hello Health University for the company. It will educate physicians who are about to launch their own practices using the platform. The tool will provide the physicians with assistance on everything creating a business, deciding whether to hire staff, and purchasing office space.
Cash-based practices
The company will offer the platform to physicians free of charge and collect a fee for each transaction.
"If physicians aren't seeing patients on the platform, they're not paying for anything," says Khozin. "If they see a patient and a transaction occurs, then a percentage of that goes to Myca/Hello Health."
The Brooklyn Hello Health office is operating a cash-based, concierge practice, since most insurers do not pay physicians for the phone, e-mail, video chat, or instant messaging services that they offer. A concierge practice allows patients to pay for this service themselves, and many patients are more than happy to do so for the added convenience of being able to access their healthcare provider. The Brooklyn practice does not accept insurance, but they will provide paperwork for patients who want to submit claims for reimbursement.
Moore says that Hello Health is one of the few venues where practices are able to completely cut loose of all the rules and impediments, allowing them to perform e-care when it makes sense because they don't need to worry about receiving reimbursement from an insurer.
Initially, Moore expressed concern that some patients may skimp on vaccines, tests, and the like if they participated in a cash-only practice. "There are a lot of people who think that if you care about healthcare, then you'll get out your wallet and pay for it," he says. "I don't think that applies to everyone."
His concern was assuaged when he learned that the platform allows physicians to determine their own price structure and payment policies. Even physicians who cater to vulnerable populations such as the uninsured, unemployed, or underserved can opt to charge as little as $25 per transaction.
"There are wonderful programs that are cash-based and accessible to a huge slot of the population," says Moore. "What I was initially interpreting as concierge, breaks open to a pretty full practice model. Those who can afford it can be a very large slot of the population depending on how you set up the pricing."
According to Moore, the company has plans to incorporate back-end billing into the platform in the future so that practices can use the platform to bill insurance companies.
A practice platform for physician "entrepreneurs"
According to Khozin, many physicians from across the country have contacted Hello Health to express an interest in using the platform for their practices. It has selected approximately 20 physicians to become part of their beta test.
"We're starting a process to educate and empower other doctors to start using the platform so they can lower their overhead and start practicing medicine in a more meaningful way," he says. "Right now, not only are patients unhappy, but a lot of doctors are unhappy. Their overhead is so high, they have to see 30 to 40 patients a day to stay afloat."
Khozin says if physicians can lower their overhead, cut down on the number of unnecessary visits, and conduct virtual visits instead, then they can have more meaningful interactions with patients and, as a result, operate a sustainable medical practice.
"They can lower their overhead, better communicate with patients, and generate more revenue," he says.
Physicians interested in the platform generally have an entrepreneurial spirit, says Khozin. The platform appeals to physicians who want to build stronger relationships with their patients to deliver effective care—something most physicians want but find difficult to achieve due to the administrative work they must complete to receive reimbursement from third parties.
"This allows a viable way of actually running a practice and making a living," says Khozin. "The traditional way has become very abrasive."
Cynthia Johnson is the editor of Medicine On The 'Net, a monthly newsletter from HealthLeaders Media.
"The health system has been moving in the wrong direction," says Sean Khozin, MD, MPH. "People talk about healthcare reform, but no one is talking about what happens between a doctor and a patient. We have to pay much closer attention to the way that doctors and patients interact and transact and enhance that process because that's where care is delivered."
Khozin's futuristic Brooklyn, NY-based practice is unlike any other. It is powered by Hello Health, a secure, Web-based platform that includes a practice management system, an electronic medical records system, and a social networking tool that allows physicians to communicate with patients both online and face-to-face. Another Hello Health practice is scheduled to open in the West Village. Both practices serve as the beta testing grounds for the product, which was developed in collaboration with a Quebec-based technology company called Myca.
Creating improved access to care
After a patient establishes a relationship with a Hello Health doctor, he or she can use e-mail, video chat, instant messaging, or phone to reach their physician to ask questions, obtain test results, and to conduct other matters which would typically require an appointment in the office.
"We establish a relationship with a patient and we do a lot of the follow ups and care coordination online," says Khozin. "We cut down on the number of unnecessary visits while giving patients different channels of communication with their doctor."
Patients still have the option of scheduling an appointment if they have a problem that requires attention, but he has found that most of the time he can conduct patient follow up visits remotely.
While not all patients feel comfortable using technology to communicate with their physicians, Khozin says they learn over time and with his encouragement. He expects that more and more people will begin relying on technology to communicate with healthcare professionals.
While video-chatting with your physician may sound out of the ordinary now, Khozin predicts that it a few years it will be commonplace for a large segment of the population. In fact, today's young generation will more than likely expect this type of communication in the future because of the way that they have embraced technology and integrated it into their lives.
For example, the company is conscious of how popular smart phones have become. According to an April report by Manhattan Research, the number of physicians using smart phones more than doubled to 64% over the past year. In response to this growing trend, the company is in the process of developing applications for use on the Apple iPhone to address the needs of patients and physicians who want to communicate using smart phones.
"A smart, health IT company builds products for devices that people already have."
Khozin currently uses his iPhone to e-prescribe, review test results, e-mail, and graph and trend disease information for patients while they are in the office.
He says that with diabetes and heart disease on the rise, physicians need to engage patients and pull them into the process of care by allowing them to use online tools to better track their health and communicate information remotely.
For example, patients with diabetes would be able to submit their glucose levels online to Hello Health and have their physician monitor their results and respond to them if necessary—all without an office appointment.
"We can't rely on office visits alone anymore," he says. "Even if you have a chronic disease and you see your doctor four times a year, the rest of the time you're on your own. By connecting a doctor virtually with a patient, you can ensure continuity of care."
Building a Hello Health "ecosystem"
When physicians conduct an in-office or remote transaction with a patient, it automatically becomes part of that patient's electronic medical record in the Hello Health platform. The patient can view their medical record at any time. In addition, other physicians in the practice who see the patient and have access to the system can also view the same information.
The company plans to develop regional "ecosystems" on the Hello Health platform that will consist of a group of primary care doctors and specialists who can communicate with the patient and with one another in a patient-centered environment. Khozin says that specialists are beginning to participate in the Hello Health platform in New York and he expects similar ecosystems to be launched throughout the country.
"There's a lot of ways this technology can be implemented in terms of coordinating the care of complex patients, such as cancer patients," he says. "It's so difficult to really take care of these patients because of lack of access to the right information when you need it."
An elegant platform to replace Frankenstein systems
L. Gordon Moore, MD, a family medicine physician, has been waiting for a product like Hello Health to come along for quite some time. He is credited with pioneering the Ideal Medical Practice (IMP) philosophy. Physicians who subscribe to IMP concepts operate low-overhead, high-technology practices that provide patient-centered care that is efficient, effective, and accessible.
To run these types of practices, physicians often piece together many different pieces of technology to build a grassroots version of what Hello Health now offers. They pull together billing systems, appointment schedulers, and bare bones EMR applications to come up with a complete, albeit imperfect, package.
"Other docs have picked up this Frankenstein system, and it's hard," he says. "They're pouring money into IT to finesse this Holy Grail of interoperability, which is almost an illusion."
By comparison, Moore describes Hello Health as an "elegant platform." "It manages relationships like nothing I've ever seen," he says. "It's really the best IT solution that I've seen out there so far."
Moore is in the process of developing Hello Health University for the company. It will educate physicians who are about to launch their own practices using the platform. The tool will provide the physicians with assistance on everything creating a business, deciding whether to hire staff, and purchasing office space.
Cash-based practices
The company will offer the platform to physicians free of charge and collect a fee for each transaction.
"If physicians aren't seeing patients on the platform, they're not paying for anything," says Khozin. "If they see a patient and a transaction occurs, then a percentage of that goes to Myca/Hello Health."
The Brooklyn Hello Health office is operating a cash-based, concierge practice, since most insurers do not pay physicians for the phone, e-mail, video chat, or instant messaging services that they offer. A concierge practice allows patients to pay for this service themselves, and many patients are more than happy to do so for the added convenience of being able to access their healthcare provider. The Brooklyn practice does not accept insurance, but they will provide paperwork for patients who want to submit claims for reimbursement.
Moore says that Hello Health is one of the few venues where practices are able to completely cut loose of all the rules and impediments, allowing them to perform e-care when it makes sense because they don't need to worry about receiving reimbursement from an insurer.
Initially, Moore expressed concern that some patients may skimp on vaccines, tests, and the like if they participated in a cash-only practice. "There are a lot of people who think that if you care about healthcare, then you'll get out your wallet and pay for it," he says. "I don't think that applies to everyone."
His concern was assuaged when he learned that the platform allows physicians to determine their own price structure and payment policies. Even physicians who cater to vulnerable populations such as the uninsured, unemployed, or underserved can opt to charge as little as $25 per transaction.
"There are wonderful programs that are cash-based and accessible to a huge slot of the population," says Moore. "What I was initially interpreting as concierge, breaks open to a pretty full practice model. Those who can afford it can be a very large slot of the population depending on how you set up the pricing."
According to Moore, the company has plans to incorporate back-end billing into the platform in the future so that practices can use the platform to bill insurance companies.
A practice platform for physician "entrepreneurs"
According to Khozin, many physicians from across the country have contacted Hello Health to express an interest in using the platform for their practices. It has selected approximately 20 physicians to become part of their beta test.
"We're starting a process to educate and empower other doctors to start using the platform so they can lower their overhead and start practicing medicine in a more meaningful way," he says. "Right now, not only are patients unhappy, but a lot of doctors are unhappy. Their overhead is so high, they have to see 30 to 40 patients a day to stay afloat."
Khozin says if physicians can lower their overhead, cut down on the number of unnecessary visits, and conduct virtual visits instead, then they can have more meaningful interactions with patients and, as a result, operate a sustainable medical practice.
"They can lower their overhead, better communicate with patients, and generate more revenue," he says.
Physicians interested in the platform generally have an entrepreneurial spirit, says Khozin. The platform appeals to physicians who want to build stronger relationships with their patients to deliver effective care—something most physicians want but find difficult to achieve due to the administrative work they must complete to receive reimbursement from third parties.
"This allows a viable way of actually running a practice and making a living," says Khozin. "The traditional way has become very abrasive."
Cynthia Johnson is the editor of Medicine On The 'Net, a monthly newsletter from HealthLeaders Media.